Glaucoma
What is Glaucoma?
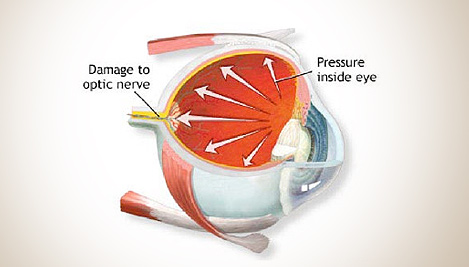
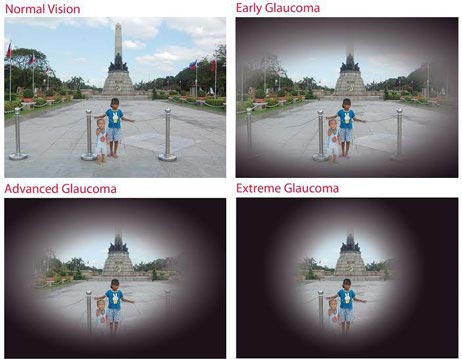
Glaucoma is an eye condition which affects the ability of the eye to send picture to the brain interfering with a persons vision.
This can be due to the optic nerve being affected, increased eye pressures damaging the nerve or both. This damage is permanent but if detected early further damage can be minimised.
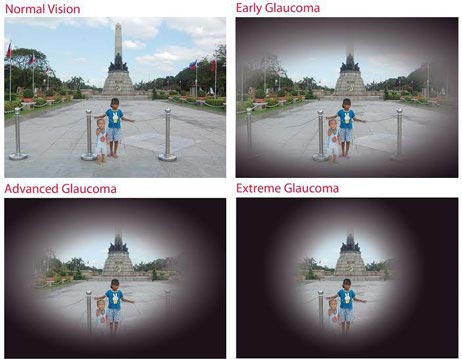
Glaucoma is painless, gradual and people often find it difficult to notice. This is because the brain automatically “fills in” gaps in the visual picture which are caused by Glaucoma. This can prevent people seeing objects or obstacles.
Only about half of the people who have Glaucoma are even aware that they have the condition. When Glaucoma develops, usually you do not have any early symptoms and the disease progresses slowly. In this way Glaucoma can steal your sight very gradually. Glaucoma can cause blindness if it is left untreated.
Fortunately, early detection and treatment (with Glaucoma eye drops, Glaucoma surgery or both) can help preserve your vision.
Types of Glaucoma
The main categories of Glaucoma include:
- Open angle Glaucoma
- Normal tension Glaucoma
- Closed angle Glaucoma (or narrow angle Glaucoma or angle closure Glaucoma)
- Secondary Glaucoma
Open Angle Glaucoma

The most common form of Glaucoma is called primary open angle Glaucoma. It occurs when the trabecular meshwork of the eye gradually becomes less efficient at draining fluid.

As this happens, your eye pressure, called intraocular pressure (IOP), rises. Raised eye pressure leads to damage of the optic nerve. Damage to the optic nerve can occur at different eye pressures among different patients.
Typically open angle Glaucoma has no symptoms in its early stages and your vision remains normal. As the optic nerve becomes more damaged blank spots begin to appear in your field of vision. You usually will not notice these blank spots in your day to day activities until the optic nerve is significantly damaged and these spots become large. If all the optic nerve fibres die, blindness results.
Normal-tension Glaucoma
Eye pressure is expressed in millimetres of mercury (mm/Hg).
Although normal eye pressure is considered a measurement less than 21 mm/Hg, this can be misleading. Some people have a type of Glaucoma called normal tension, or low tension Glaucoma. Their eye pressure is consistently below 21 mm/Hg, but optic nerve damage and visual field loss still occur. People with normal tension Glaucoma typically receive the same methods of treatment used for open-angle Glaucoma.
Conversely, ocular hypertension is a condition where someone has higher eye pressure than normal, but does not have other signs of Glaucoma, such as optic nerve damage or blank spots that show up in their peripheral (side) vision when tested. Individuals with ocular hypertension are at higher risk for developing Glaucoma later relative to those with lower or average eye pressure. Just like people with Glaucoma people with ocular hypertension need to be closely monitored by an Ophthalmologist to ensure they receive appropriate treatment.
Closed-angle Glaucoma
A less common form of Glaucoma is closed angle. Closed angle Glaucoma occurs when the iris (the coloured part of the eye) partially or completely blocks off the drainage angle of the eye. Unlike open angle Glaucoma eye pressure usually goes up very fast. People with hyperopia (farsightedness) tend to be more at risk for developing this form of Glaucoma.
If the drainage angle becomes completely blocked eye pressure rises quickly resulting in a closed angle Glaucoma attack. Symptoms of an attack include:
- Severe eye or brow pain
- Redness of the eye
- Decreased or blurred vision
- Seeing coloured rainbows or halos
- Headache
- Nausea
- Vomiting
A closed angle Glaucoma attack is a medical emergency and must be treated immediately. Unfortunately, people at risk for developing closed angle Glaucoma often have few or no symptoms before the attack.
People at risk for closed angle Glaucoma should avoid over the counter decongestants and other medications where the packaging states not to use these products if you have Glaucoma.
Secondary Glaucoma
Secondary Glaucoma is Glaucoma that results from another eye condition or disease. For example, someone who has had an eye injury, someone who is on long term steroid therapy or someone who has a tumour may develop secondary Glaucoma.
Risk factors for Glaucoma include:
- Age
- Family history of Glaucoma
- African or Hispanic ancestry
- Farsightedness or nearsightedness
- Elevated eye pressure
- Past eye injury
- Having a thinner central cornea (the clear, front part of the eye covering the pupil and coloured iris)
- Not having eye examinations when they are recommended
- Conditions that affect blood flow, such as migraines, diabetes and low blood pressure
Below is a list of tests that may be performed:-
Tonometry Exam.
This procedure measures the pressure in your eye. During this exam, your eyes are numbed with eye drops. Mr. Golchin uses an instrument called a tonometer to measure eye pressure. The instrument measures how your cornea resists to pressure.
Gonioscopy Exam.
Gonioscopy allows Mr. Golchin to get a clear look at the drainage angle of your eye. Mr. Golchin is not able to see your eyes drainage by looking at the front of your eye, however by using a mirrored lens, he can examine the drainage angle, which is important in determining whether or not you have Glaucoma, as well as what type of Glaucoma you may have.
Ophthalmoscopy Exam.
Your optic nerve is inspecte d for signs of damage using an ophthalmoscope, an instrument that magnifies the interior of the eye. Your pupils will be dilated (widened) with eye drops to allow a better view of your optic nerve to see if it is has been damaged.
d for signs of damage using an ophthalmoscope, an instrument that magnifies the interior of the eye. Your pupils will be dilated (widened) with eye drops to allow a better view of your optic nerve to see if it is has been damaged.
Visual Field Test
The visual field test will check for blank spots in your vision, another sign of Glaucoma. The test is performed using a bowl shaped instrument called perimeter. When taking the test, a patch is temporarily placed on  one of your eyes so that only one eye is tested at a time. You will be seated and asked to look straight ahead at a target. The computer makes a noise and random points of light will flash around the bowl shaped periemter and you will be asked to press a button whenever you see a light. Not every noise is followed by a flash of light.
one of your eyes so that only one eye is tested at a time. You will be seated and asked to look straight ahead at a target. The computer makes a noise and random points of light will flash around the bowl shaped periemter and you will be asked to press a button whenever you see a light. Not every noise is followed by a flash of light.
OCT (Optical Coherence Tomography)
Optical coherence tomography (OCT) is a non-invasive imaging test. OCT uses light waves to take cross-section pictures of your retina.
With OCT, your ophthalmologist can see each of the retina’s 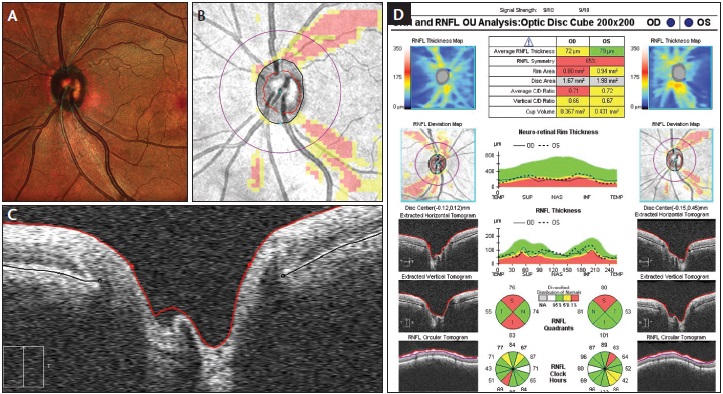 distinctive layers. This allows your ophthalmologist to map and measure their thickness. These measurements help with diagnosis and treatment guidance for glaucoma. It can also be used to detect other retinal diseases such as ARMD (Age Related Macular Degeneration) and Diabetic Eye Disease.
distinctive layers. This allows your ophthalmologist to map and measure their thickness. These measurements help with diagnosis and treatment guidance for glaucoma. It can also be used to detect other retinal diseases such as ARMD (Age Related Macular Degeneration) and Diabetic Eye Disease.
Pachymetry
Because the thickness of the cornea can affect eye pressure readings, pachymetry is used to measure corneal thickness. A probe called a pachymeter is gently placed on the cornea to measure its thickness.
Treatment of Glaucoma
There is no cure for Glaucoma but treatments are available which can help stop the progression of the disease.
How your Glaucoma is treated will depend on your specific type of Glaucoma, the severity of your disease and how it responds to treatment.
Medicated eyedrops are the most common way to treat glaucoma. These medications lower your eye pressure.
These eyedrops must be taken regularly every day as prescribed by Mr. Golchin. Never change or stop taking your medications without talking with your doctor.
 Selective Laser Trabeculoplasty (SLT)
Selective Laser Trabeculoplasty (SLT)
Laser surgery has become increasingly popular as an alternative method of treating pressure. Selective Laser Trabeculoplasty (SLT) is a relatively new laser treatment for open angle glaucoma. SLT uses short pulses of low energy laser light to target melanin containing cells in a network of tiny channels, called the trabecular meshwork. The objective of the procedure is to help fluids drain out of the eye, reducing intraocular pressure that can cause damage to the optic nerve and loss of vision.
The selective technique is much less traumatic to the eye than Argon Laser Trabeculoplasty (ALT), which has been the standard laser procedure. ALT can cause tissue destruction and scarring of healthy cells in the trabecular meshwork structure. SLT reduces intraocular pressure without this risk. SLT can be used to effectively treat some patients who could not benefit from ALT. This includes patients who have already been treated with ALT.
SLT can be given as first line treatment or as a complimentary treatment for patients already on Glaucoma drops.
Laser procedure is not a permanent solution and the effects can wear off. Up to 50% of patients have positive still maintain good control of the pressure for five years afterwards. However, if the pressure rises SLT can be repeated. Some people may need to continue using Glaucoma drops.
Medical and laser treatment can control the pressure in the vast majority of patients with Glaucoma however, a few people may require surgical treatment such as trabeculectomy or aqueous shunt surgery.





 d for signs of damage using an ophthalmoscope, an instrument that magnifies the interior of the eye. Your pupils will be dilated (widened) with eye drops to allow a better view of your optic nerve to see if it is has been damaged.
d for signs of damage using an ophthalmoscope, an instrument that magnifies the interior of the eye. Your pupils will be dilated (widened) with eye drops to allow a better view of your optic nerve to see if it is has been damaged. one of your eyes so that only one eye is tested at a time. You will be seated and asked to look straight ahead at a target. The computer makes a noise and random points of light will flash around the bowl shaped periemter and you will be asked to press a button whenever you see a light. Not every noise is followed by a flash of light.
one of your eyes so that only one eye is tested at a time. You will be seated and asked to look straight ahead at a target. The computer makes a noise and random points of light will flash around the bowl shaped periemter and you will be asked to press a button whenever you see a light. Not every noise is followed by a flash of light.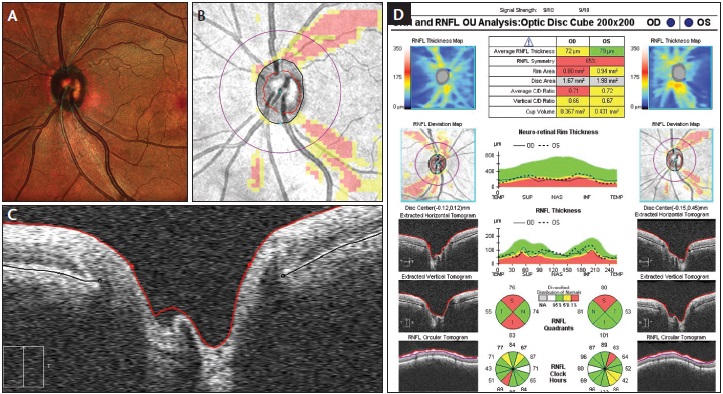 distinctive layers. This allows your ophthalmologist to map and measure their thickness. These measurements help with diagnosis and treatment guidance for glaucoma. It can also be used to detect other retinal diseases such as ARMD (Age Related Macular Degeneration) and Diabetic Eye Disease.
distinctive layers. This allows your ophthalmologist to map and measure their thickness. These measurements help with diagnosis and treatment guidance for glaucoma. It can also be used to detect other retinal diseases such as ARMD (Age Related Macular Degeneration) and Diabetic Eye Disease.

 Mr. Behrooz Golchin
Mr. Behrooz Golchin